What
future treatment is recommended?
NIH
Response |
Ongoing surveillance
for antimicrobial resistance is crucial to obtain the information needed
to choose effective treatments for gonorrhea. The decreasing susceptibility
of Neisseria gonorrhoeae to fluoroquinolones has raised questions
about the use of these antibiotics to treat uncomplicated gonorrhea in
light of the recent reports of antimicrobial failures and in vitro evidence.
It is important that these future treatments do not inhibit the absorption
of fluoroquinolones, since this can greatly effect therapeutic outcomes,
not allowing for optimal therapy (CTR, 1997). |
Bambeke and
Tulkens (1999) recommend the following when considering local epidemiology
and the indication of fluoroquinolone use:
The use of the fluoroquinolones should
focus on infections in which
-
There is a differential benefit over conventional
agents in terms of efficacy, safety, or cost;
-
in infections for which few alternative
treatments exist, or
-
against organisms towards which they are
sufficiently active to prevent the rapid emergence of resistance.
| In
1997, Mroczkowski et al. determined
that a single oral dose of grepafloxacin is an effective fluoroquinolone
antibiotic used to treat uncomplicated gonorrhea, and proved to be effective
even against penicillinase-producing gonococci; this can be added to the
list of other fluoroquinolones currently approved by the CDC: ciprofloxacin,
ofloxacin, enoxacin and norfloxacin.
The authors stated that it had excellent in vitro activity and is more
potent than ofloxacin against penicillin- and tetracycline-resistant strains,
and claimed it to be more effective than ceftriaxone and ofloxacin against
Chlamydia
trachomatis and penicillinase-producing N. gonorrhoeae (Mroczkowski,
et al., 1997). |
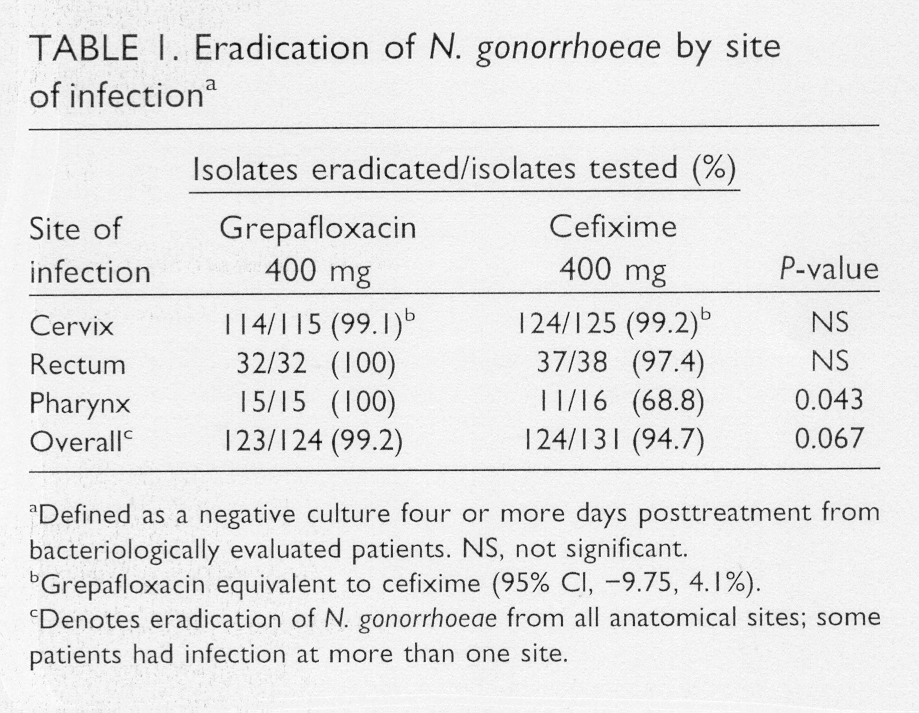
Grepafloxacin
Effectiveness
|
In 1998,
Jones
et
al. determined that a new quinolone antibiotic, trovafloxacin,
is highly active in vitro against uncomplicated gonorrhea, even against
strains that showed mild resistance to ciprofloxacin and ofloxacin.
It is also active against Chlamydia trachomatis, since many individuals
with gonorrhea concurrently are infected with chlamydia, along with numerous
other Gram positive and Gram negative bacteria.
Jones
et
al. determined that these resistance phenotypes included ones that
were pencillin-susceptible; chromosomally mediated resistance to pencillin
and tetracycline; penicillinase-producing N. gonorrhoeae and those
strains with plasmid-mediated resistance because of the TetM determinant;
and plasmid-mediated resistance to tetracycline.
As of 1999, no
clinically significant resistance to the broad-spectrum cephalosporins
have been identified, and fluoroquinolone-resistant gonococcal strains
are now prevalent in Australia and much of the Far East (Fox
and Knapp, 1999).
Due to the convenience
of single oral doses, effectiveness in males and females, safety profile,
and relatively low cost, trovafloxacin and ofloxacin remain the preferred
quinolone treatments for uncomplicated gonorrhea when compared to ceftriaxone,
an effective but costly injectible (Jones et
al., 1998). However, grepafloxacin did have a higher percentage
of adverse side-effects with 25.7% (Mroczkowski,
et al., 1997) compared to the findings of Jones et al. which
was 10% lower for each antibiotic.
It is yet to be seen whether these two
fluoroquinolones, grepafloxacin and trovafloxacin, will be useful for a
significant period of time. Nonetheless, the research and development
of new fluoroquinolone antimicrobial agents is imperative for the treatment
of N. gonorrhoeaea, and other Gram positive cocci, such as S.
pneumoniae and methicillin-sensitive
S. aureus, as well as atypical
pathogens of the respiratory system like Chlamydia, Legionella,
and Mycoplasma (File and Slama, 2000).
Home
Next
Previous