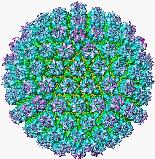
ACYCLOVIR (ACV)
Chemical Structure (Pielop et al.)
HSV is most commonly treated with antiviral therapies because studies have shown the efficacy of them in reducing the duration and severity of genital and oral herpes.. There are two different approaches to antiviral management of HSV, both of which depend wholly on the nature of the disease, lifestyle and psychosocial consideration. These include "episodic" oral antiviral therapy (where antiviral therapy is used intermittently by the patient during a recurrence), or "suppressive" antiviral therapy (where the antiviral therapy is taken continuously to prevent recurrences) (Miller, AHMF).
ORAL HERPES (HSV-1)
Primary oral-facial HSV infections are usually
diagnosed as gingivostomatitis or pharyngitis and are seen in young children
or adults. The first antiviral cream to be approved for cold sores
was penciclovir (Denavir). It heals sores about one day faster than
without treatment, stops viral shedding, and reduces the amount and duration
of pain associated with blisters. One study showed that foscarnet
(Foscavir) reduced the size of the blisters and increased the rate of healing
when HSV-1 was induced by intense sunlight. Another study showed
that an ointment composed of caffeine and interferon (a component of the
immune system) increased healing time compared to using the interferon
alone. A new antiviral therapy, Ascoxal, a solution applied to the
sores with a cotton ball, is composed of ascorbic acid (Vitamin C) and
substances that fight the typical symptoms associated with the oral virus--it
is showing promise (WebMD).
Acyclovir (ACV, more information in next section), the primary antiviral
therapy used in HSV-2 infections, has not been found to be entirely beneficial
for recurring eruptions; however, it is used, quite successfully, for severe
primary eruptions. Oral antiviral therapies may be effective, but
they are not FDA approved for use in oral-facial herpes infections.
This is due to the fact that chronic topical application of ACV cream has
proved ineffective in the suppression of recurrences, although oral ACV
has been somewhat successful.
GENITAL HERPES (HSV-2)
ACYCLOVIR (ACV)
Chemical
Structure (Pielop et al.)
|
Molecules "R" Us |
Conversion of acyclovir to acyclovir triphosphate leading to DNA chain termination |
Inhibition of HSV (Pillay) |
VALACYCLOVIR (VAL)
Chemical Structure (Pielop
et
al.)
Valacyclovir, a valine ester prodrug of ACV, has a bioavailability three to five times that of ACV. This antiviral drug is rapidly converted to ACV after oral consumption, resulting in higher plasma ACV concentrations than those of oral ACV, comparable to those of IV ACV. Because of this, VAL can be taken orally twice daily as opposed to five daily doses of ACV. One study compared oral VAL 1000mg twice daily versus ACV 200mg five times daily for 10 days. Both courses of antiviral treatment were equally effective, according to the FDA. At the end of the experiment, however, it was determined that a one dose improvement over the ACV 400mg three time daily dosage commonly prescribed by physicians is more expensive. It is thought that the decreased dosage frequency may improve compliance and thus ultimately clinical efficacy (Pielop et al., 2000).
FAMCICLOVIR (FAM)
Chemical Structure (Pielop
et
al.)
Famciclovir,
oral form, undergoes extensive first-pass metabolism to penciclovir (PCV,
a nucleoside analogue that has a similar mechanism of action as ACV) after
consumption, reaching maximum levels in less than an hour if taken while
fasting. PCV has been shown to be effective against a small percentage
of acyclovir-resistant HSV strains in vitro (Lazarus
et
al., 1999). FAM has an improved bioavailability
(77%, compared to ACV's 20%), and significantly longer intracellular half-life
in its PCV triphosphate form (10-20 hours, compared to ACV's triphosphate
form of 1 hour). This allows for less frequent dosages. VAL
and FAM are similar in their high absorption and bioavailability, safety
profile, and efficacy in treating primary episodes of genital herpes.
FAM is often prescribed 250mg three times daily for 5-10 days to treat
primary primary infections, but it is not FDA approved for this usage
(Pielop et al., 2000).